The applications of 3D printing in dentistry have created a change in basic assumptions in how we deliver clinical care to our patients. The technology now offers a wide variety of potential uses across prosthodontics, implantology, oral and maxillofacial procedures, orthodontics, endodontics, and periodontics.
Despite some limitations in printing accuracy and quality, 3D printing in dentistry has become increasingly widespread, allowing us to produce dental solutions faster and at lower costs. From creating highly customized implants that perfectly fit a patient's anatomy to serving various purposes in endodontic procedures such as access cavity preparation and apicoectomy, this technology makes life easier not just for dental providers like us but also delivers significant benefits to our patients through customized, affordable dental solutions.
In this comprehensive guide, we will explore the various 3D printing technologies currently available, including stereolithography, digital light processing, fused deposition modeling, and more. We will also examine the materials used and the specific applications across dental specialties, helping you understand how this digital revolution is transforming our industry.
3D printing technologies in dentistry have evolved remarkably over the past decade, offering various methods to fabricate dental components with unprecedented precision. Each technology has unique principles, advantages, and applications that meet different needs in dental practice. Let us go through the main technologies that are shaping modern dental care.
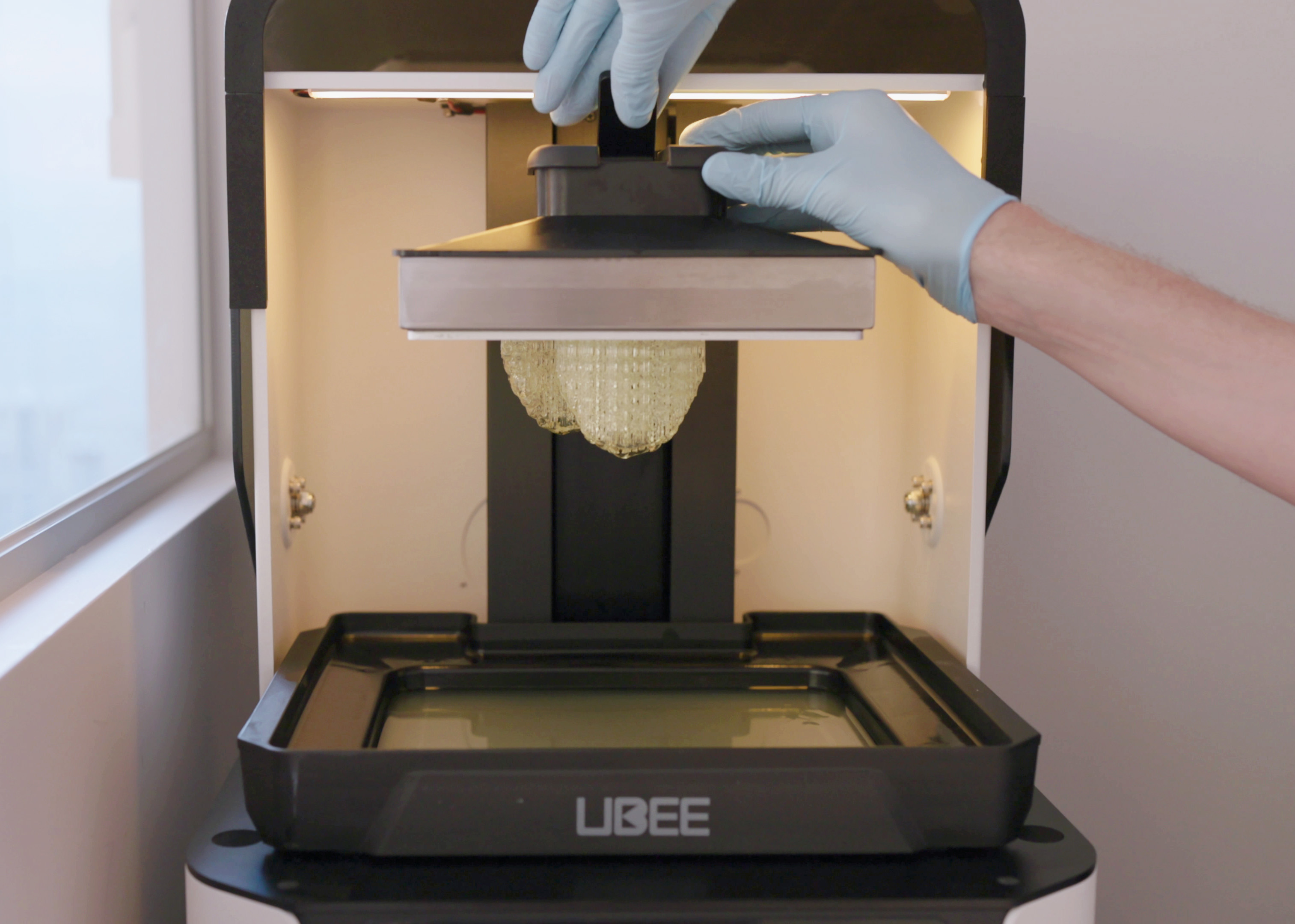
Stereolithography stands as the oldest and most widely utilized 3D printing technique in dentistry [1]. This technology employs an ultraviolet (UV) laser to cure a liquid photopolymer resin layer by layer. During the process, a vat holds liquid resin while the laser precisely polymerizes each layer it contacts. After creating one layer, the build platform descends slightly, allowing subsequent layers to form on top of previous ones [1].
The advantages of SLA printing include impressive speed, high resolution, relatively low cost compared to other 3D printer types, and the ability to construct intricate designs [1]. Furthermore, high-end SLA printers can produce a wide range of dental products, from orthodontic aligners and surgical guides to splints, occlusal guards, complete dentures, and even temporary and permanent crowns [1].
SLA produces parts with superior surface finishes and fine features, making it a good option for smooth surface quality [2]. Additionally, the technology creates watertight objects with continuous geometries—a critical feature for dental applications where air or fluid flow must be precisely controlled [2].
DLP shares similarities with SLA in curing and polymerization techniques but differs in its light source—utilizing a digital projector instead of a laser [1]. This difference enables DLP to polymerize an entire material layer simultaneously in the x-y axis, significantly increasing fabrication speed for large-scale printing jobs [1].
While faster than SLA for larger or multiple objects, DLP typically trades speed for slightly lower resolution and surface detailing on large prints. However, when build volume is reduced, resolution improves considerably [1]. This is the reason why some manufacturers offer larger and smaller build plates for their 3D printers. One not able drawback involves voxel lines that create small rectangular steps affecting curved edges, which often require post-manufacturing modification through sandblasting or special fusing agents [1].
Despite these challenges, DLP achieves excellent feature resolution down to several micrometers on small-scale printing jobs, making it ideal for products requiring extreme accuracy like complete and partial dentures, thermoform models, surgical guides, and multi-unit wax-ups [1].
FDM operates on material extrusion principles, where thermoplastic material in filament form is pushed through a heated nozzle that melts the material [3]. The nozzle moves along a programmed path, depositing the melted material onto a platform. Once one layer completes, the platform lowers to allow for subsequent layer formation [3].
In dentistry, FDM offers advantages through its relatively low cost and wide material selection, including PLA, PETG, ABS, PVA, TPU, and specialty filaments doped with metals or carbon fiber [3]. Nevertheless, FDM typically produce slower resolution outputs (200-500 μm) compared to other dental printing technologies, making it less suitable for high-precision applications [4].
Current applications include occlusal appliances and controlled-release delivery systems, though its use remains limited in clinical dentistry [5].
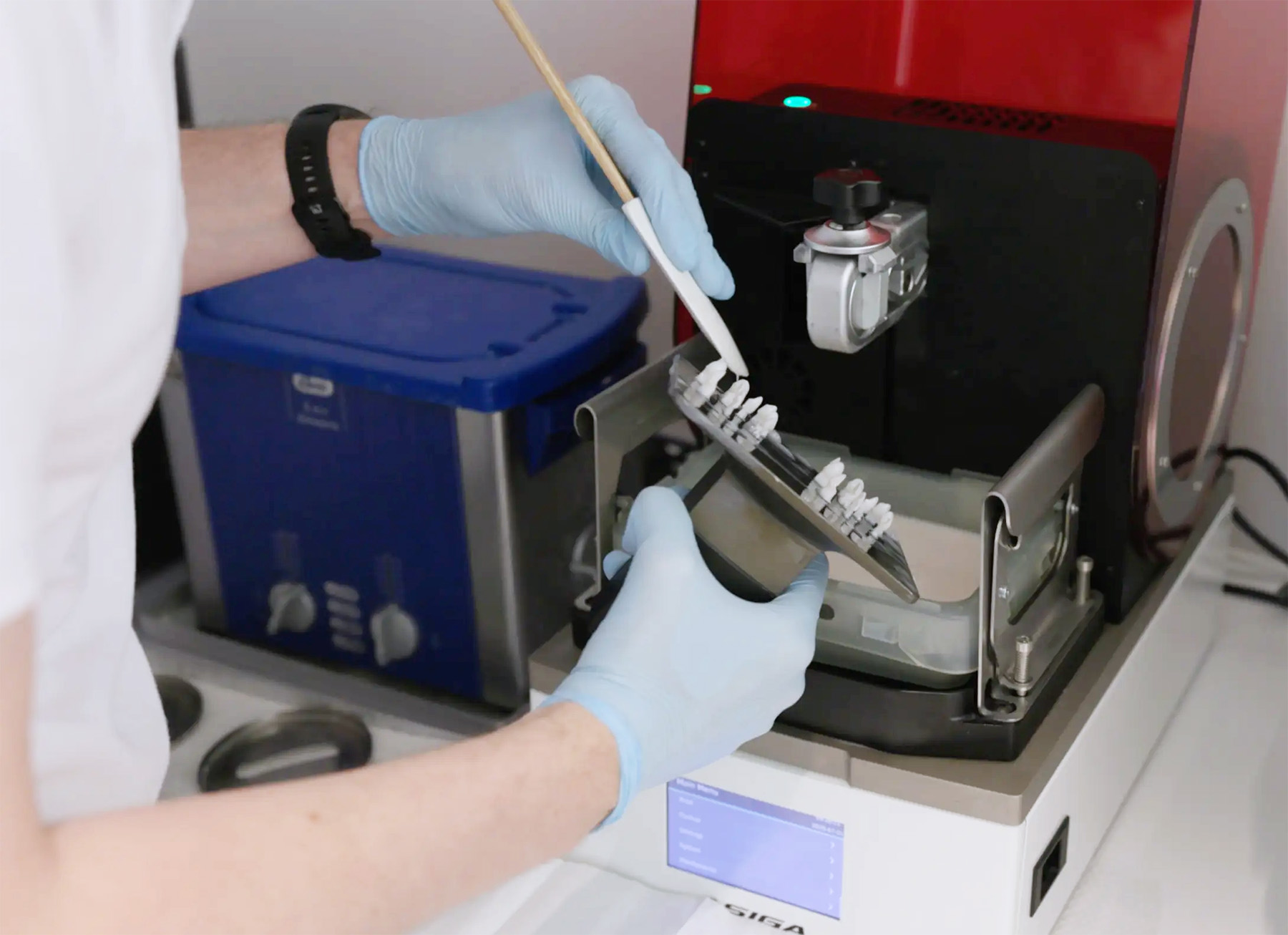
Selective laser sintering and selective laser melting have become essential for fabricating metal components in dentistry. These technologies use high-temperature lasers to selectively fuse or melt powdered materials—including ceramics, metals, and polymers [5].
The primary distinction between SLS and SLM lies in the material state during processing: SLS partially melts (sinters) the powder particles while SLM completely melts them [5]. Both technologies offer significant advantages for dental applications requiring high-density materials.
SLS/SLM have demonstrated remarkableresults in fabricating removable partial denture frameworks, significantly reducing human error compared to traditional casting techniques [5]. Moreover, studies comparing SLM-produced Co-Cr dental prostheses with conventional casting found that additive manufacturing yielded higher hardness values [6].
Material jetting (MJ) operates similarly to household inkjet printers, depositing light-sensitive polymer through printer nozzles and curing it via UV light one layer at a time [1]. This technology produces objects with accuracy equal to SLA and small-batch DLP printers without requiring post-manufacturing modifications [1].
A unique advantage of material jetting is its ability to print multiple colors or even materials simultaneously in a single print cycle. These materials can vary in biomechanical properties, and textures—making it highly versatile for esthetically complex cases [1].
One example of material jetting currently available is the use of trial dentures during the diagnostic and fitting phases of prosthodontic treatment. With its capacity for multi-material and multi-color printing, the technology enables precise simulation of gingival tones and tooth shades, as well as fine detailing of occlusal surfaces and tissue contours. These lifelike trial dentures allow patients to visualize and experience their future prosthesis before final fabrication, improving aesthetic evaluation and functional testing, and streamlining adjustments for the definitive appliance.
Laser-assisted bioprinting utilizes a laser as an energy source and consists of an energy-absorbing layer, a donor ribbon, and a receiving substrate [1]. This nozzle-free, non-contact technology can deposit high-viscosity bioinks with excellent resolution without concerns about nozzle clogging [1].
LAB maintains exceptionally high cell viability during printing (>95%) [8], though the long-term effects of laser exposure on cells remain under investigation [1]. The technology has shown promising applications in producing tissue-engineered constructs for periodontal regeneration, bone augmentation, and oral mucosal reconstruction [5].
The success of dental 3D printing depends largely on selecting the right materials for specific clinical applications. As materials science advances, we now have access to a diverse range of printable substances that meet the rigorous demands of dental practice.
Resin-based materials, particularly light-curable methacrylate and acrylate formulations, play a pivotal role in high-resolution dental 3D printing methods such as Stereolithography (SLA) and Digital Light Processing (DLP). These resins begin as liquid photopolymers that solidify layer by layer when exposed to specific wavelengths of light—typically ultraviolet (UV) or visible blue light—initiating a polymerization reaction. The process forms robust cross-linked polymer networks with excellent dimensional stability and surface quality. Resin materials are widely used for fabricating crowns, bridges, surgical guides, and dental models, thanks to their smooth finish, fine detail reproduction, and tunable physical properties. Post-curing under controlled light and temperature conditions enhances their mechanical performance and ensures biocompatibility for intraoral applications.
Polymeric materials remain another option for dental 3D printing due to their versatility and tunable properties. Polymethyl methacrylate (PMMA) serves as a predominant foundation for dentures, temporary crowns, bridges, obturators, and retainers [9]. Despite its cost-effectiveness and stability in the oral environment, PMMA possesses limited mechanical properties and high shrinkage rates during curing. To enhance its performance, researchers have incorporated nanodiamonds, PEEK, TiO2, SiO2, and Al2O3 as reinforcement [10].
Polylactic acid (PLA) has gained popularity as an eco-friendly alternative compatible with Fused Deposition Modeling techniques [9]. Its applications span orthodontic devices, surgical guides, and temporary restorations. Still, PLA's low glass transition temperature (55-60°C) restricts its use primarily to temporary or non-loaded applications [11]. One solution involves blending PLA with PMMA, which has shown promising results with 13.24% and 19.07% higher flexural and compression strengths compared to neat PLA materials [12].
Polyether ether ketone (PEEK) stands out for its excellent mechanical and chemical resistance, high biocompatibility, and lightweightness [10]. Nonetheless, being bioinert, PEEK lacks osseointegration capabilities. Researchers have addressed this limitation through surface modifications and the addition of bioactive hydroxyapatite, ceramic nanoparticles, and carbon fibers [10].
Metal alloys play a crucial role in dental applications requiring strength and durability. Titanium alloy (Ti6Al4V or TC4) and cobalt-chromium-molybdenum (CoCrMo) represent the primary metals used in dental 3D printing.
Titanium alloy features approximately half the density of cobalt-chromium (4.42 g/cm³ vs. 8.30 g/cm³), creating lightweight restorations that improve patient comfort [2]. Its thermal conductivity—only one-sixth that of cobalt-chromium—protects dental pulp from temperature fluctuations. Especially noteworthy, titanium's elastic modulus (110±10 GPa) most closely resembles human hard tissue, offering superior resilience in clinical settings [2].
For applications requiring exceptional wear resistance, CoCrMo alloys excel with their impressive hardness (400±5 HV5) and tensile strength (1270±50 MPa) [2]. The chromium component forms a protective oxide layer against corrosion, whereas molybdenum enhances strength and corrosion resistance [13]. Notably, research has found that 3D-printed CoCrMo abutments demonstrate comparable fit to CNC-milled versions [14].
Ceramic materials have revolutionized esthetic dental restorations. Zirconia-based materials, particularly 3Y-TZP (3 mol.% yttria-stabilized tetragonal zirconia polycrystal), offer outstanding properties including high flexural strength, excellent ionic conductivity, thermal stability, and corrosion resistance [15].
The transformation toughening mechanism represents zirconia's most remarkable property—under stress, the metastable tetragonal phase transforms to monoclinic, expanding by approximately 4.5% and creating compression that retards crack growth [15]. This property contributes to 3D-printed zirconia materials achieving impressive Vickers hardness values up to 13.4±0.2 GPa and bending strengths exceeding 800 MPa [16].
Aluminum oxide (alumina) serves as another vital ceramic in dental applications, featuring higher hardness than zirconia albeit with lower fracture toughness. In 3D printing workflows, alumina allows for extremely thin wall thicknesses (0.15 mm) and through-holes with comparable diameters [17].
Biocompatibility remains a primary concern for all dental materials. Titanium alloy demonstrates superior cytocompatibility compared to cobalt-chromium, which shows certain cytotoxicityto human gingival fibroblast cells [2]. Among polymers, extensive research indicates variability in biocompatibility, with some formulations exhibiting cell-friendly properties while others demonstrate cytotoxicity [18].
Essentially, post-processing significantly impacts material safety and performance. Studies indicate that ethanol post-treatment ameliorates toxicity in 3D-printed objects [18]. Additionally, proper washing protocols and UV post-curing reduce monomer leaching by tightening polymer chains and enhancing the overall degree of conversion [19]. For optimal biocompatibility, the elimination of double bonds, attainment of a fully solid resin state, and removal of excess liquid resin through appropriate post-processing prove critical [19].
From digital impressions to final restorations, 3D printing has found its way into every dental specialty. Let's explore the diverse clinical applications that are transforming dental practice.
Digital workflows in prosthodontics have been revolutionized with 3D printing technology. Complete and partial denture scan now be fabricated directly from digital designs without traditional molding techniques, reducing patient visits and improving precision [20]. 3D-printed dentures demonstrate flexural strength values of 96 MPa for the base and 110 MPa for the teeth, comparable to conventional options [21]. For crowns and bridges, studies have shown that 3D-printed restorations exhibit better internal and marginal fit (141.1 μm and 91.1 μm respectively) compared to milled alternatives (171.6 μm) [22].
Surgical guides for implant placement represent one of the most common 3D-printed applications, offering unprecedented accuracy and safety. Research shows guided implant placement results in average deviations of less than 1 mm at both the implant entry point and apex [3], significantly improving upon free-hand implantation which shows errors of 2.5 mm at the apex [3]. Additionally, the angular deviation improves from 9.8° with free-hand to just 4.2° with guided placement [3]. Some designs now incorporate coolant channels that reduce bone temperature during drilling to 2.1°C compared to 3.2°C with standard guides [3].
In orthodontics, 3D printing enables production of custom aligners with increased efficiency. Direct-printed aligners (DPAs) offer better fit and precision with customized pressure points [23]. Likewise, 3D-printed retainers have proven accurate and reliable compared to vacuum-formed alternatives [4]. Furthermore, custom orthodontic auxiliaries like specialized chains for impacted teeth can be printed, offering better bonding and compliance [4].

For maxillofacial reconstruction, 3D printing facilitates surgical planning and execution through anatomical models, cutting guides, and patient-specific implants. These guides ensure precise placement of bone segments [24], reducing operative time and enhancing outcomes. Patient-specific titanium implants and biocompatible polymers like PEEK are increasingly used for reconstructing complex defects [25].
Access cavity preparation and apicoectomy procedures benefit from 3D-printed guides, with reported angular deviations of less than two degrees [26]. For periodontal applications, biocompatible scaffolds facilitate tissue regeneration, offering greater reduction in pocket depth and improved bone fill [27].
Accurate dental models created through 3D printing serve as foundations for various indirect procedures, including diagnosis, treatment planning, and patient education [28]. These high-quality models enable dental professionals to visualize complex oral anatomies, simulate clinical outcomes, and communicate treatment options clearly to patients, ultimately improving clinical decision-making and patient satisfaction.

3D-printed bleaching trays provide custom-fit with precise reservoirs and excellent marginal sealing, preventing substantial gel leakage and gum irritation [6]. This technology ensures more efficient whitening by keeping the bleaching gel exactly where it belongs—on the teeth [6].
Dental veneers produced through 3D printing offer exceptional accuracy and fit. Using FDA-approved dental-specific resins, these permanent tooth coverings require minimal preparation while delivering natural esthetics [29]. Consequently, digital smile design allows patients to preview results before treatment, facilitating better-informed decisions [30].
In examining the practical impact of 3D printing, we must weigh both its revolutionary benefits and ongoing limitations in clinical dental practice.
First and foremost, 3D printing enables the creation of highly personalized dental products. Traditional impressions often cause discomfort and may not always produce perfect molds. In contrast, digital scans create exact replicas of patients' dentition, ensuring more accurate fits [31]. This precision reduces adjustment need safter placement and enhances overall patient comfort. The technology's ability to produce complex shapes and geometries—otherwise infeasible with traditional methods—represents a significant advantage [26]. Beyond esthetics, customization improves treatment outcomes as 3D-printed dental devices integrate more seamlessly with Speed and Workflow Efficiency patients' natural anatomy.
Regarding treatment time, 3D printing dramatically reduces traditional waiting periods. Many dental devices can now be produced in hours rather than days [32], allowing for same-day treatments in certain cases. This efficiency benefits both dental professionals and patients through fewer appointments and adjustments. For dental labs, the digital workflow from scanning to design to printing minimizes errors while enhancing production consistency [32]. Indeed, studies show that additive methods require only 90 minutes to produce 10 crowns, compared to 450 minutes for subtractive methods and 930 minutes for conventional production [33].
On balance, although initial equipment investments remain quite substantial, particularly for smaller practices [34], 3D printing offers significant long-term economic advantages. Research indicates 3D printing is 5.5, 8.7, and 10.2 times less expensive than PMMA, milled composite, and lithium disilicate production, respectively [35]. For a dental office producing 10 aligner models daily, in-house printing becomes more economical than outsourcing after just seven weeks, potentially saving over $40,000 annually [5].
Despite advancements, limitations persist in printing accuracy and surface quality. Layer thickness significantly impacts precision—thicker layers create greater inaccuracies [7]. Different technologies show varying accuracy levels: PolyJet demonstrates the lowest root mean square error (0.145±0.10 mm), followed by DLP (0.161±0.12 mm) and SLA (0.345±0.23 mm) [7]. Surface roughness differs with printing orientations, particularly notable with DLP technology [36]. For clinical acceptance, the maximumcritical value is ±0.25 mm, representing the threshold for creating orthodontic movement [7].
The integration of 3D printing technologies has undoubtedly transformed modern dentistry. Throughout this article, we have explored how various printing methods—from stereolithography and digital light processing to fused deposition modeling and laser bioprinting—are changing our approach to patient care. These technologies, paired with an expanding range of biocompatible materials such as polymers, metals, and ceramics, have opened new possibilities across all dental specialties.
Dental practitioners now benefit from unprecedented precision and efficiency. 3D-printed surgical guides ensure implant placement with deviations under 1 mm, while custom prosthetics fit more accurately than traditional alternatives. Additionally, the digital workflow reduces treatment time dramatically, producing ten crowns takes merely 90 minutes compared to 450 minutes with subtractive methods.
Cost considerations remain significant, though long-term economics favor 3D printing. Despite substantial initial investments, the technology proves 5 to 10 times less expensive than conventional production methods for many applications. This cost advantage becomes particularly evident for practices producing multiple items daily.
Certain limitations still exist, particularly regarding accuracy and surface quality. Different printing technologies demonstrate varying precision levels, with layer thickness significantly impacting the final results. Nevertheless, researchers continue addressing these challenges through improved materials and post-processing techniques.
Looking ahead, 3D printing will certainly become even more integral to dental practice. The technology will likely advance toward faster production speeds, greater material options, and improved biocompatibility. Most importantly, these developments will continue benefiting our patients through more comfortable, precise, and affordable dental care. Though still evolving, 3D printing has fundamentally changed dentistry—creating better outcomes one layer at a time.
At Sweeth, we understand that getting started with 3D printing can feel overwhelming. That’s why we make it simple — bringing together hardware, validated materials, software, and expert support into one seamless all-in-one solution.
✅ Advice on materials (specializing in aligners)
⚙️ Optimization and assistance with setup and 3D printing
🔄 Workflow support from scan to print
🎓 Training & ongoing support for you and your team
Why choose Sweeth? We don’t just sell printers and materials – we deliver a working workflow! Sweeth guides you through the entire process to ensure your transition to in-house printing goes smoothly.
[1] - https://pmc.ncbi.nlm.nih.gov/articles/PMC9504181/
[2] - https://www.eplus3d.com/comparison-of-3d-printing-tc4-and-cocrmo-material-in-dentistry.html
[3] - https://pmc.ncbi.nlm.nih.gov/articles/PMC10603942/
[4] - https://pmc.ncbi.nlm.nih.gov/articles/PMC10318848/
[5] - https://dental.formlabs.com/blog/dental-3d-printer-price/
[6] - https://www.dentamile.com/en/software/new-bleaching-tray-workflow
[7] - https://pmc.ncbi.nlm.nih.gov/articles/PMC11705190/
[8] - https://pmc.ncbi.nlm.nih.gov/articles/PMC10140526/
[9] - https://pmc.ncbi.nlm.nih.gov/articles/PMC11598508/
[10] - https://pmc.ncbi.nlm.nih.gov/articles/PMC9460687/
[11] - https://www.nature.com/articles/s41598-023-44150-2
[12] - https://4spepublications.onlinelibrary.wiley.com/doi/10.1002/pen.26829?af=R
[14] - https://pubmed.ncbi.nlm.nih.gov/37847843/
[15] - https://pmc.ncbi.nlm.nih.gov/articles/PMC10004380/
[16] - https://jbioleng.biomedcentral.com/articles/10.1186/s13036-023-00396-y
[17] - https://www.caddent.de/en/blog/3d-printing-ceramic-material
[18] - https://pmc.ncbi.nlm.nih.gov/articles/PMC10839546/
[19] - https://www.mdpi.com/2073-4360/16/19/2795
[20] - https://pmc.ncbi.nlm.nih.gov/articles/PMC6262086/
[21] - https://glidewelldental.com/solutions/removable-prosthesis/dentures/simply-natural-digital-dentures
[22] - https://pmc.ncbi.nlm.nih.gov/articles/PMC11031267/
[23] - https://www.sciencedirect.com/science/article/pii/S1073874624001178
[24] - https://pmc.ncbi.nlm.nih.gov/articles/PMC9651252/
[25] - https://www.tandfonline.com/doi/full/10.2217/3dp-2022-0025
[26] - https://pmc.ncbi.nlm.nih.gov/articles/PMC10814684/
[27] - https://pmc.ncbi.nlm.nih.gov/articles/PMC6906903/
[29] - https://newportbeachdentalstudio.com/3d-printed-dental-veneers/
[30] - https://www.colgate.com/en-us/oral-health/veneers/3d-printed-dental-veneers
[33] - https://www.mdpi.com/2673-1592/7/4/78
[35] - https://www.sciencedirect.com/science/article/pii/S0022391322004814
[36] - https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-024-05365-5
July 30, 2025
Jens Linard
Industry Insights
Learn how 3D printing enhances dental treatments across prosthodontics, implants, surgery, and orthodontics, improving accuracy and patient experience.